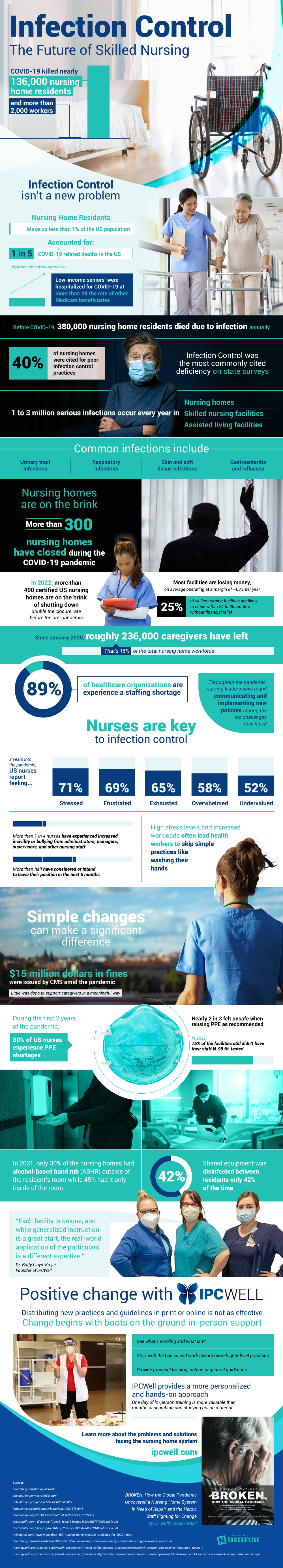
Nursing homes shouldered the brunt of the damage during the pandemic, revealing long-standing issues with infection control in skilled nursing facilities. COVID-19 killed over 135,000 nursing home residents and more than 2,000 workers, yet nursing home residents make up less than 1% of the United States population. In total, nursing home residents accounted for 1 in 5 COVID-19-related deaths in the U.S. In addition to older residents disproportionately dying due to COVID-19, there were economic disparities among this population; low-income seniors eligible for both Medicare and Medicaid were hospitalized for COVID-19 at more than four times the rate of any other Medicare beneficiaries.
The Pandemic Impact on Nursing Homes
Not only did COVID-19 impact nursing homes by death rate, but it also contributed to staffing shortages. In the healthcare field since January 200, over 235,000 caregivers have left the field; that number is 15% of the total nursing home workforce. More than one-quarter of nurses have experienced increased incivility or bullying from administrators, managers, supervisors, and other nursing staff, and more than half of nurses have considered or intend to leave their position in the next 6 months. Two years into the pandemic, nurses in the United States report feeling a range of negative emotions about their work environments. Namely, 71% of nurses report feeling stressed and 69% report feeling frustrated. Over half of nurses reported feeling undervalued as well.
Nurses are essential to infection control, and less favorable work environments heavily impact these practices. Before the pandemic, 380,000 nursing home residents died due to infection annually. Nursing homes, skilled nursing facilities, and assisted living facilities are where 1 to 3 million serious infections occur every year. Infection control was the most commonly cited deficiency on state surveys for care facilities; almost half of the nursing homes were cited for poor infection control practices. After the pandemic, these numbers have gotten worse.
Hope for a Recovery?
Nursing homes are on the brink following the pandemic. More than 300 nursing homes have closed during the COVID-19 pandemic, and in 2022, more than 400 certified U.S. nursing homes are on the verge of shutting down. This is double the closure rate pre-pandemic, illustrating the impact the pandemic had on these facilities. On top of this, most facilities are losing money – on average operating at a margin of almost -5% annually. In the future, 25% of skilled nursing facilities are likely to close within 24 to 36 months if they don’t receive financial relief.
Little was done to support caregivers in a meaningful way during the pandemic, affecting sanitation practices. During the first two years of the pandemic, 80% of nurses experienced PPE shortages and nearly 2 in 3 felt unsafe when reusing PPE as recommended. In 2021, only 30% of the nursing homes had alcohol-based hand rub outside of the resident’s room while 45% had it only inside the room. Additionally, shared equipment was disinfected between residents only 42% of the time.
In Conclusion
Throughout the pandemic, nursing leaders have found communicating and implementing new policies among the top challenges they faced. Simple changes can make a significant difference, and distributing new practices and guidelines with on-the-ground in-person support is the best way to facilitate these changes. Through an in-person program, strategists can see what’s working and what isn’t and provide practical training instead of general guidelines. It’s important to have a a personalized and hands-on approach to learning more about the problems and solutions facing your nursing home system.
Source: IPCWell.com







 WebProNews is an iEntry Publication
WebProNews is an iEntry Publication